MIDWIFE
Farah Kanj
Midwife
Waterbirth certified
Prenatal & postnatal support
Pelvic Floor assessment & recovery
Farah is a certified midwife and a certified waterbirth provider. She graduated from the Lebanese University in 2005, with a degree in Midwifery. She has a particular interest in pelvic floor health and has completed multiple courses in pelvic floor rehabilitation.
Farah moved back to Beirut in 2017, after living abroad for more than 10 years. After having 3 kids of her own and experiencing natural birth and VBAC, she became an advocate of women choosing to give birth differently. After working with several NGOs on women and child health programs, Farah saw an opportunity to make an impact in women’s journeys. Farah currently works on birth support, providing prenatal and postnatal services, homebirth, water birth and pelvic floor rehabilitation.
Badaro, Beirut
Phone:+9613603689
Email: farah@holisticmidwife.net
a.holistic.midwife a.holistic.midwife

introduction
Your pregnancy can be a special time for you. It can also be a confusing time, when you are not sure what the right thing to do is. This is especially true these days, with so much conflicting information on the internet. This guide is intended to help you to be proactive about your birth, to be confident in sharing your concerns with your health care provider and to get involved in the decision-making process. After all it is your birth!
You can do many things to prepare for the birth process ahead of time. The more prepared you are mentally and physically, the better your experience and memories of the process will be.
This guide will help you to prepare and look after yourself during pregnancy, birth, labor and beyond. One important way you can prepare to give birth is by preparing your pelvic floor.
The pelvic floor is important in our daily life as it is a major part of our core muscle group. The pelvic floor can be thought of as a hammock at the base of your core that holds all of our pelvic organs. After birth, the pelvic floor may be compromised due to the stressors of pregnancy and/or labor.
Not taking care of our pelvic floor could lead to several complications, such as leaking urine or prolapse. Therefore, it is important that women are equipped with the knowledge needed to understand the role of the pelvic floor and how to keep it strong and healthy.
Pelvic floor
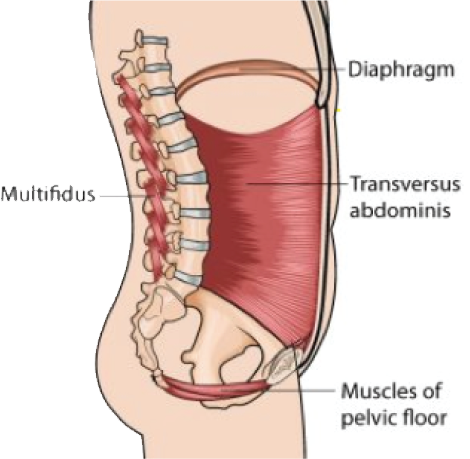
The pelvic floor is a term used to describe the group of muscles at the base of your pelvis. Your pelvic floor muscles are part of your core, which is a system of four groups of muscles: the diaphragm at the top, the abdominals or transversus abdominus towards the front, the back muscles or multifidus at the back and the pelvic floor at the bottom. These muscles work in harmony to help us to move, breathe, give birth and to do most of our daily chores and activities.
The core: the pelvic floor is like a hammock at the bottom of your pelvis the pelvic floor lies like a hammock or sling below your pelvis. It passes around and between your urethra (where you pass urine) through your vagina to your anus (where you pass a bowel motion). The nerves, muscles and connective tissues in this area work together to maintain our bladder and bowel function, to provide support for our internal organs (uterus, bladder and rectum) and to stabilize our spine and pelvis.
The pelvic floor is the foundation of our core and it deserves a lot more attention than it gets.
What happens when those
muscles don’t work properly?
Pelvic floor dysfunction
Pelvic floor challenges can result from overuse or underuse of the muscles, which can happen during pregnancy and labor. Two of the most common types of pelvic floor dysfunction are:
Incontinence
- Incontinence is the involuntary loss of urine or feces (poo). Incontinence can refer to bladder function (urinary incontinence) or rectal function (fecal incontinence). It can have many causes, namely: weakened muscles, overused muscles or poor timing of muscle contractions. %50 of women will experience urinary incontinence at some point in their life and %33 will develop regular problems. Incontinence is more common in women who have had children.
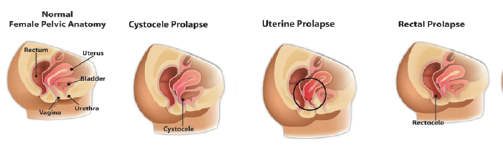
Prolapse
- Prolapse is the descent of one or several of the pelvic organs through the vaginal opening. The severity of prolapse varies, and is measured in degrees, from 1 to %50 .5 of women who have had children will have some degree of prolapse. Most women who suffer from prolapse are unaware of it due to the fact that there are few symptoms in the early stages. With pregnancy, birth, aging and changes in hormone levels, prolapse can evolve in severity.
Prolapse can happen to any of the three pelvic organs:
- Uterus, which is called uterine prolapse;
- Bladder, which is called cystocele;
- Rectum, which is called rectocele.
50% of women who have diastasis recti (the separation of the abdominal muscles that occurs in pregnancy due to the stretching of those muscles) will have some pelvic floor dysfunction (mainly incontinence or prolapse).
It should be noted that prolapse does not only occur in women who have had children.
Is there a solution?
Luckily, there are ways to prepare your body to lessen your risk of complications like incontinence and prolapse, by looking after your pelvic floor. There are exercises women (and men) can do to strengthen their pelvic floor and avoid complications.
How to find your pelvic floor?
Imagine you need to use the toilet or pass wind; the muscles you tense to stop yourself are your pelvic floor muscles. You might find it easier to find your pelvic floor muscles while lying down or standing instead of sitting. Find what works for you.
Contracting your pelvic floor muscles is often called a Kegel exercise, or Kegels.
Doing Kegels right after birth allows more blood flow into the pelvic area which will accelerate the healing process. Practicing Kegel exercises while pregnant will strengthen and prepare your pelvic floor for labor and birth.
If you suffer from tightness, pelvic pain or movement restrictions, Kegels might not be for you!
We only recommend Kegels when you have consulted your health professional. Your health professional can help you learn to engage, contract and relax your pelvic floor.
Some tips regarding your pelvic floor (applicable to every stage of your life):
- Avoid exercises that make you leak such as jumping, running and weight lifting until your function has been restored and then gradually return to that activity.
- Tighten your pelvic floor muscles before you cough, sneeze or lift heavy items.
- Avoid constipation. Repeated straining is similar to mini childbirth for your pelvic floor, which can cause these muscles to become weak over time.
- Don’t urinate when you don’t really need to; learn to wait until your bladder is full before going to the bathroom. You should urinate 5-9 times a day.
- Drink water consistently throughout the day. Restricting fluids can cause your urine to become concentrated, which can irritate your bladder and signal you to empty more often than you should.
- Pay attention to your menstrual cycle. Estrogen levels change throughout your monthly cycle, and this affects your pelvic floor. Right before, during, and right after your period is generally when your estrogen levels are at their lowest, making you more likely to experience leakage during that time.
- Avoid bladder irritants like artificial sweeteners, acidic foods, chocolate, alcohol and caffeine.
- Share with your daughters, sisters, aunts, friends—all women need to know this information!
Preparing your birth plan preferences:
Preparing a birth plan is a way for you to educate yourself on your options. It will help you to choose the options that suit you and are in line with your birth philosophy. Do your research and discuss it with your birth provider ahead of time to go through the options and agree on the details. The support of a partner is of great value because he/she will be the one reminding the hospital staff of your preferences and ensuring that you are getting what you had envisioned for your birth. You have the right to choose a partner that you believe will provide you with the support you need. The birth plan doesn’t have to be complicated; it can be simple and straight to the point.
Here are some points that you can research and include in your birth plan:
- Having your own music
- Dimming the lights
- Moving while in labor
- Intermittent monitoring
- Having an IV
- Number of vaginal checks
- Rupture of the water or keeping it intact
- Waiting for the urge to push
- Birth positions
- Episiotomy
- Skin to skin contact
- Delayed cord clamping
- Rooming in
- Delaying baby’s bath
There are plenty of templates online, you can browse and choose one that suits you or you can make your own. Here’s a sample that I find very easy to read and implement.
We always plan for birth, but just like anything in life our plans might not always work out, which is why we call these preferences. We should always be grateful for medical advancement and its interference in times of need.

Labor
Labor is when your body starts working in harmony to produce effective contractions that will lead to the birth of your baby.
Try to invite the contractions in as they are what gets the baby out!
For some, labor starts with the rupture of water, for others with a little bleed/mucus and for others with contractions. At first, contractions are short and irregular and the pain is bearable. No need to rush to the hospital. Early labor can take quite some time, especially for first time parents (sometimes up to 24 hours), so if you are low-risk, you can stay home in early labor (after consulting with your doctor or midwife). When the contractions become regular, longer and more intense, you have reached active labor and this is when you should head to the hospital. Active labor will require you to really focus, so some women prefer dim lights, less visitation and no noise in this phase.
Arriving to the hospital during active labor will limit unnecessary interventions and increase the chances of natural delivery. As the contractions become stronger and more painful, remember to breathe, deal with one contraction at a time, do not think about the other ones that may come.
Make sure to rest in between contractions, take a deep breath, a sip of water, maybe a bite to eat. Release the contraction all the way and rest when possible. Move as much as you can, walk and squat (see diagram below for recommended positions during labor). If you are lying down, place a peanut ball or lots of pillows between your legs to keep the pelvis open for your baby to move down and rotate. Don’t push before you are fully dilated, as this will increase pressure and strain on the pelvic floor muscles. Breathe…
When in labor a woman is at her most vulnerable, and she may agree to things that are asked even if they weren’t in her birth plan or preferences. This is when her team (partner, doula, midwife) should play their role of supporting and advocating for her and making sure her needs/wishes are being met.

These positions are recommended by the Royal College of Midwives (United Kingdom).
One of the most important tips for labor is to trust your body and remember that birth is a normal, natural and physiological process. Most of the time it proceeds normally without any intervention when there is proper support.
Birth
Childbirth is a long process that usually ends with your happy, healthy baby in your arms. It is the only time where pain is productive! Thinking about the contractions of labor being productive will help you to understand and tolerate the pain. Discomfort from contractions means that your cervix is changing, dilating and getting ready to let your baby out into the world. When your cervix is fully dilated and your baby has passed the pelvic griddle, it’s time for you to push. You will feel it! My best advice is to listen to your body and push when you’re ready. Preparing ahead of time will pay off greatly during birth. Your pelvic floor muscles will help the baby to rotate and make its descent into the birth canal. Your breath, coupled with a strong core, will help you to push effectively.
You will be emotional at this stage. It’s very normal to feel that you cannot think clearly, and this is when you most need support. The pushing phase might last anywhere from a couple of minutes to a couple of hours and this is affected by many factors:
- Your position. The lying down position that we often see works against gravity. While it might be the best position for the healthcare provider to see what is happening, it might not be the best position for the woman giving birth. Ask your provider about different birth positions; you can choose squatting, lying on your side, staying on all fours, and many others;
- The baby’s position;
- The readiness of your core and the quality of your pushes.

Breastfeeding
Breastfeeding comes naturally to some women but it doesn’t to everyone. It needs commitment and patience, especially in the first couple of weeks until you establish milk supply. Breastfeeding is also a time when you can practice your Kegels (if needed), as well as some of the exercises that are allowed during the first couple of weeks (consult with a pelvic floor specialist/midwife first).
My golden rule is to establish skin-to-skin contact immediately after birth. Before you get the baby dressed put him straight on your chest under your gown, and cover yourself to preserve heat. Skin-to-skin contact will increase the secretion of oxytocin, which will help the uterus contract back to its previous shape and avoid post-partum hemorrhage. It will also stimulate milk production. Dad can also help in skin-to-skin in case mom is tired.
Your skin (smell, heart beat) will give your baby
– who has been inside your womb for 9 months
– a sense of security and familiarity.
Other than establishing a good initiation for breastfeeding, skin-to-skin also helps with:
- Stabilizing the baby’s body temperature;
- Regulating the baby’s blood sugar;
- Improving heart and lung functions;
- Ensuring the transfer of good bacteria from mom to baby;
- Easing the baby’s transition from the womb;
- Boosting mother-child bonding.
Your baby’s stomach is very small, growing gradually as they grow. Whatever amount of colostrum your body produces during the first couple of days are what your baby needs. Don’t forget they also have to get used to digesting their own food. After all, you were providing all of their nutrition through the umbilical cord and placenta before this. Colostrum is the baby’s best first food, it’s easy to digest and has super antibodies to boost and help to build their immune system.
Here is a picture of the size of a newborn’s stomach up until one month of age.
Breastfeeding shouldn’t hurt. When there is pain that continues throughout the feed consult with a lactation consultant, you don’t have to go through it alone! The most common challenges are the position of the baby and the latch. A lactation consultant can help you to correct those and save you a lot of money on formula later on!

Take care of yourself so that you can take care of your baby
- Educate yourself from trusted sources, read books and take prenatal workshops. This is the only way for you to know your options and choose what suits you best and what is in your best interest.
- Watch lots of birth videos and familiarize yourself with the sight and sounds of birth. Watch loud ones, quiet ones, messy ones, clean ones, water ones. WATCH THEM ALL WITH SOUND UP!
- Avoid hearing traumatic birth stories! Fear is your enemy, you want to go to your birth with a mind equipped with knowledge and anticipation and a body equipped with a strong pelvic floor. You do not want fear and worries!
- Nutrition is paramount, so eat healthy wholesome food. Fresh fruits and vegetables are essential to your diet, they’re packed with nutrients and vitamins much-needed in pregnancy and will give you strength and energy for birth.
- Exercise as much as your health permits. Exercise is beneficial on so many levels during pregnancy. It keeps you energized and fit, and it lifts your mood. It is also beneficial for birth, providing you with the strength and flexibility you need for the baby’s passage in the birth canal. After birth, it helps you to recover faster and gives you the strength you need to take care of yourself and your baby.
- Don’t forget to stretch your pelvic floor muscles in particular. Stretching is very beneficial to your pelvic floor; it will lengthen the muscles and prepare them for the heavy work of labor and ease the recovery phase.
As Maya will help you to regain your muscle strength, I can help you to regain your pelvic floor function and make your motherhood an enjoyable journey!
Testimonials

Seza Movsesian
I've been following Maya since 2017, I was a new mom back then, with extra Kgs. ...
Read more


